Case Studies
Peripartum Cardiomyopathy – A typical case

Dr Kemi Tibazarwa
A female patient [M.M.] presented at Chris Hani Baragwanath Hospital with a 5 week history of shortness of breath equivalent to New York Heart Association Functional Class II, orthopnoea associated with cough, bilateral leg swelling, and mild dizziness.
The patient presented one week after she underwent spontaneous vaginal delivery; the symptoms thus having begun 4 weeks prior to term delivery.
On further interrogation, there was positive family history of sudden “unexplained” death and this patient was neither a smoker nor did she consume alcohol.
Clinical examination revealed bilateral pitting pre-tibial oedema, and jugulo-venous pressure raised by up to 3cm. The pulse rate was 92 per minute, irregular, weak, and blood pressure 97/72mmHg. On palpation the apex beat was displaced laterally, and the abdominal exam proved there to be tender hepatomegaly. On cardiac auscultation positive findings include a loud split second heart sound, and loud systolic murmur best heard over mitral and tricuspid areas. The arrhythmia was suspected to be one of ventricular extrasystoles. Chest auscultation proved there to be bilateral basal crepitations,
Chest x-ray demonstrated 4-chamber cardiomegaly and pulmonary congestion, while her ECG showed right axis deviation, with diffuse T-wave inversion, and non-sustained ventricular ectopics. Positive 2-dimensional echocardiography findings have been illustrated below, including dilatation of all 4 chambers, poor systolic left ventricular function, mild functional mitral regurgitation, severe tricuspid regurgitation with resultant severe pulmonary hypertension, and a small clear pericardial effusion. The ejection fraction, as estimated from the fractional shortening of 20.8%, was 41.7%. Tissue-doppler imaging revealed no evidence of diastolic function.
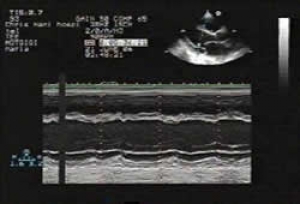
Fig.1: 2-dimensional transthoracic echocardiography (TTE) with long axis parasternal view and M-Mode showing three dilated chambers and poor LV systolic function. |
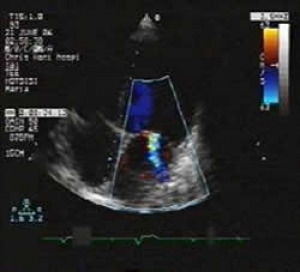
Fig.2: 2-dimensional TTE in long axis 4-chamber view showing all four dilated chambers and functional mitral regurgitation |
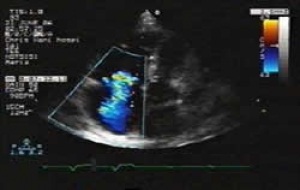
Fig.3a: 2-dimensional TTE showing tricuspid regurgitation |
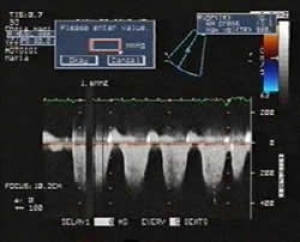
Fig.3b: Continuous-wave Doppler across the previous image demonstrating pulmonary hypertension |
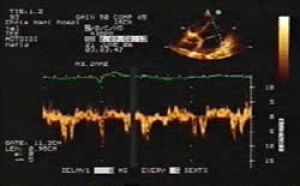
Fig.4: Tissue-doppler imaging with lateral Ea-wave velocities falling just within that of normal diastolic function. |
Treatment was initiated using Carvedilol, Enalapril, Aldactone, Slow K, and Lasix therapy, and the symptoms subsided within a week. Management and follow-up of the patient continue.The patient was booked for a spiral CT scan, and further tests permitted the exclusion of other commom causes of dilated cardiomyopathy, as well as important differential diagnoses. The workimg diagnosis remained that of peripartum cardiomyopathy.
